Histamine Intolerance & the Microbiome
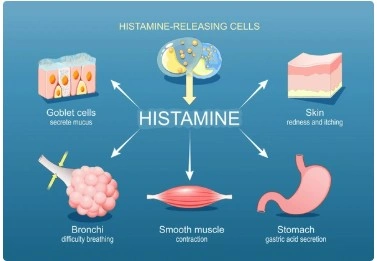
Histamine intolerance is the term used to describe a range of symptoms attributed to excess histamine due to the inability to eliminate histamine. Histamine intolerance is difficult to diagnose due to the overlap of symptoms with other conditions, the variety of presentations, and the lack of diagnostic testing.
Symptoms of Histamine Intolerance:1
Bloating
Constipation
Diarrhea
Abdominal pain
Shortness of breath
Nasal congestion
Sneezing
Headache/migraine
High heart rate
Flushing
Itchy skin
Rashes/hives
It is important to note that histamine intolerance presents in a variety of different ways. Most people do not have all the symptoms and it can look differently in different people. For example, for some people, it may present primarily with skin issues whereas other people may have only digestive symptoms. This can make this condition more difficult to spot.
There are a few recognized causes of histamine intolerance, though much more research is needed to understand this condition.
One of the primary issues may be around the enzyme diamine oxidase (DAO). DAO is expressed in the small intestine where its job is to break down histamine from food. DAO can be deficient or not function correctly. Research has identified multiple mutations in the gene for DAO that result in reduced function of the enzyme.1 DAO levels can be low due to medications or damage to the small intestine.1 Medications that may impact DAO include proton pump inhibitors2, NSAIDs2, some antibiotics3, some blood pressure medications2, and more3. Intestinal conditions that may result in lower DAO include IBD1, celiac disease1, non-celiac gluten sensitivity1, and SIBO6.
DAO may also be affected by copper, vitamin C, and B6 deficiency.4 And it appears that sex hormones may also influence DAO activity, leading to fluctuations in symptoms throughout the menstrual cycle.4
Outside of DAO, excess histamine levels may be caused by defects in histamine metabolism and excess histamine production by the microbiome.
Histamine & the Microbiome
Histamine intolerance may have multiple connections to the microbiome. It is important to understand that it is a two way street — low DAO and excess histamine may change the microbiome and the microbiome may contribute to excess histamine. The research has not fully teased out all the complexities so far.
SIBO bacteria can cause histamine intolerance indirectly
The first consideration is small intestine bacterial overgrowth (SIBO). SIBO can cause mucosal damage in the small intestine and decreased DAO6, leading to a transient and acquired histamine intolerance —meaning the histamine intolerance will resolve with successful treatment of SIBO. The bacteria that are commonly overgrown in SIBO may also produce histamine.9 SIBO bacteria also produce other substances that prevent histamine from being broken down in the gut and help histamine bind to mucin, thereby potentiating histamine’s effects in the gut.9 So through multiple mechanisms, SIBO can indirectly result in excess histamine in the gut.
Large intestine microbiome in histamine intolerance is different
A very small study looked at the microbiome of individuals with histamine intolerance compared to healthy individuals using 16S rRNA sequencing. Individuals with histamine intolerance had lower relative abundance of Prevotellaceae,
Alterations in DAO associated with microbiome imbalances
Another small study found that people with high serum DAO had decreased abundance of Phocaeicola, Lachnospira, Bacteroides, Alistipes, Agathobacter, Lachnospira and Bacteroides and increased abundances of Mediterraneibacter, Blautia, Faecallibacterium, Agathobacter, and Parasutterella compared to people with normal serum DAO.7
It is important to understand that DAO is found in higher amounts in the blood when there is increased intestinal permeability.7 So higher serum DAO is not a good thing—it means leaky gut. It is also important to note that this is an association, not causation. Meaning the authors did not conclude that the microbiome caused changes in DAO levels or leaky gut. Since DAO is active in the gut upstream of the large intestine microbiome, the theory is actually that changes in DAO and intestinal permeability in the small intestine may result in dysbiosis in the large intestine—so histamine intolerance may cause dysbiosis.7
Gut bacteria can produce histamine
Research has identified 117 species of bacteria with genes to produce histamine.8 Bacteria can make histamine from the amino acid histidine.8 Certain species of Bacteroides, Clostridium, Bifidobacterium, Fusobacterium, and Lactobacillus can produce histamine and are common member of the large intestine microbiome.8 Other studies have identified Enterococcus faecalis, Bifidobacterium pseudocatenulatum, Lactobacillus gasseri, Escherichia coli, Morganella morganii and Proteus mirabillis as capable of producing histamine.5
However, it appears that histamine production is very strain specific8, so do not assume that your Bacteroides produce histamine. Also, bacteria can transfer their genes to other bacteria (called horizontal gene transfer)8 so the genetics of your specific microbes may be different than what is found in the research. Just because you have Lactobacillus gasseri does not mean it makes histamine.
Gut bacteria can reduce histamine levels
Certain microbiome residents such as Clostridium perfringens, E. coli, and K, pneumoniae may be able to consume histamine, thus reducing histamine levels.10
Other microbes found in fermented foods or probiotics can also metabolize histamine. Lactobacillus plantarum D-103 degraded 100% of histamine in vitro.11 Rummeliibacillus stabekisii, Agrobacterium tumefaciens, Bacillus cereus, Bacillus polymyxa, Bacillus licheniformis, Bacillus amyloliquefaciens, and Bacillus subtilis may also degrade histamine.12 Certain strains of Brevibacterium can also degrade histamine.13
Testing/Diagnosis
There are currently no clinically validated tests for histamine intolerance and there is no consensus for a diagnostic approach - more research is needed.
To date, the research has considered serum DAO, skin prick test, histamine challenge, fecal histamine, and genetic testing, but all methods have their limitations and are not validated to diagnose histamine intolerance.
So for now, it is a clinical diagnosis, meaning that it is diagnosed based on symptoms and response to treatment.
What about assessing the microbiome for histamine production? Bottomline, there is no accurate way to do this yet. 16S rRNA sequencing cannot accurately tell you about histamine whatsoever. It is not accurate for species, and definitely not for strains. Regardless, looking at phylogeny to determine function of the microbiome is not accurate. You need to assess histamine producing gene presence and expression. 16S rRNA sequencing does not assess the presence of histamine genes. Whole genome sequencing can, but it cannot tell you about expression. Just because a gene is present does not mean it is active —it does not mean the bacteria are actually making histamine. We do not have accurate ways to assess actual histamine production throughout the small and large intestines at this time.
Treatment
For now, the gold standard of treatment is a low histamine diet. Other treatment strategies include supplementing with DAO, antihistamines, and targeted nutrient supplementation.
Modulating the microbiome may be an effective strategy to address histamine intolerance, but we need more research. Current microbiome strategies involve avoiding histamine producing bacteria in fermented foods and probiotics and supplementing with “histamine safe” probiotics. For many people, this yields only mild results, if any. As we have discussed, the microbiome may only be a small part of histamine intolerance. So just addressing the microbiome may not be enough. Furthermore, the research so far does indicate that the microbiome varies a lot amongst individuals with histamine intolerance.5,8 So for best results, microbiome treatments will need to be personalized.
References
- Jochum C. Histamine Intolerance: Symptoms, Diagnosis, and Beyond. Nutrients. 2024 Apr 19;16(8):1219. doi: 10.3390/nu16081219. PMID: 38674909; PMCID: PMC11054089.
- Tobajas Y, Alemany-Fornés M, Samarra I, Romero-Giménez J, Tintoré M, Del Pino A, Canela N, Del Bas JM, Ortega-Olivé N, de Lecea C, Escoté X. Diamine Oxidase Interactions with Anti-Inflammatory and Anti-Migraine Medicines in the Treatment of Migraine. J Clin Med. 2023 Dec 4;12(23):7502. doi: 10.3390/jcm12237502. PMID: 38068554; PMCID: PMC10707353.
- Leitner R, Zoernpfenning E, Missbichler A. Evaluation of the inhibitory effect of various drugs / active ingredients on the activity of human diamine oxidase in vitro. Clin Transl Allergy. 2014 Jul 18;4(Suppl 3):P23. doi: 10.1186/2045-7022-4-S3-P23. PMCID: PMC4127955.
- Shulpekova YO, Nechaev VM, Popova IR, Deeva TA, Kopylov AT, Malsagova KA, Kaysheva AL, Ivashkin VT. Food Intolerance: The Role of Histamine. Nutrients. 2021 Sep 15;13(9):3207. doi: 10.3390/nu13093207. PMID: 34579083; PMCID: PMC8469513.
- Sánchez-Pérez S, Comas-Basté O, Duelo A, Veciana-Nogués MT, Berlanga M, Latorre-Moratalla ML, Vidal-Carou MC. Intestinal Dysbiosis in Patients with Histamine Intolerance. Nutrients. 2022 Apr 23;14(9):1774. doi: 10.3390/nu14091774. PMID: 35565742; PMCID: PMC9102523.
- Segovia-Silvestre T, Pita AM, Vilar L, Venereo Y, Orta X, Farriol M. Intestinal ornithine decarboxylase in short bowel syndrome patients with oral diet. Clin Nutr. 2001 Apr;20(2):171-5. doi: 10.1054/clnu.2000.0369. PMID: 11327746.
- Shi L, Li Y, Liu Y, Jia H. Alterations of gut microbiota and cytokines in elevated serum diamine oxidase disorder. Medicine (Baltimore). 2022 Dec 16;101(50):e31966. doi: 10.1097/MD.0000000000031966. PMID: 36550793; PMCID: PMC9771309.
- Mou Z, Yang Y, Hall AB, Jiang X. The taxonomic distribution of histamine-secreting bacteria in the human gut microbiome. BMC Genomics. 2021 Sep 26;22(1):695. doi: 10.1186/s12864-021-08004-3. PMID: 34563136; PMCID: PMC8465708.
- Leite G, Rezaie A, Mathur R, Barlow GM, Rashid M, Hosseini A, Wang J, Parodi G, Villanueva-Millan MJ, Sanchez M, Morales W, Weitsman S, Pimentel M; REIMAGINE Study Group. Defining Small Intestinal Bacterial Overgrowth by Culture and High Throughput Sequencing. Clin Gastroenterol Hepatol. 2024 Feb;22(2):259-270. doi: 10.1016/j.cgh.2023.06.001. Epub 2023 Jun 12. PMID: 37315761.
- Pugin B, Barcik W, Westermann P, Heider A, Wawrzyniak M, Hellings P, Akdis CA, O'Mahony L. A wide diversity of bacteria from the human gut produces and degrades biogenic amines. Microb Ecol Health Dis. 2017 Jan 1;28(1):1353881. doi: 10.1080/16512235.2017.1353881. PMID: 28959180; PMCID: PMC5614385.
- Kung HF, Lee YC, Huang YL, Huang YR, Su YC, Tsai YH. Degradation of Histamine by Lactobacillus plantarum Isolated from Miso Products. J Food Prot. 2017 Oct;80(10):1682-1688. doi: 10.4315/0362-028X.JFP-17-135. PMID: 28885051.
- Lee YC, Lin CS, Liu FL, Huang TC, Tsai YH. Degradation of histamine by Bacillus polymyxa isolated from salted fish products. J Food Drug Anal. 2015 Dec;23(4):836-844. doi: 10.1016/j.jfda.2015.02.003. Epub 2015 Mar 21. PMID: 28911502; PMCID: PMC9345454.
- Leuschner RG, Heidel M, Hammes WP. Histamine and tyramine degradation by food fermenting microorganisms. Int J Food Microbiol. 1998 Jan 6;39(1-2):1-10. doi: 10.1016/s0168-1605(97)00109-8. PMID: 9562873.
Categories: dysbiosis Histamine Intolerance Tags: dysbiosis Histamine Intolerance
