Tracking Your Microbiome Over Time: What to Expect & When to Re-Test
Your gut microbiome isn’t static — it’s a living ecosystem that responds to your diet, stress, sleep, and environment. If you’re on a gut-healing or microbiome restoration program, you might be wondering:
How often should I test, and what changes should I expect to see?
Let’s break it down.
Why Track Your Microbiome?
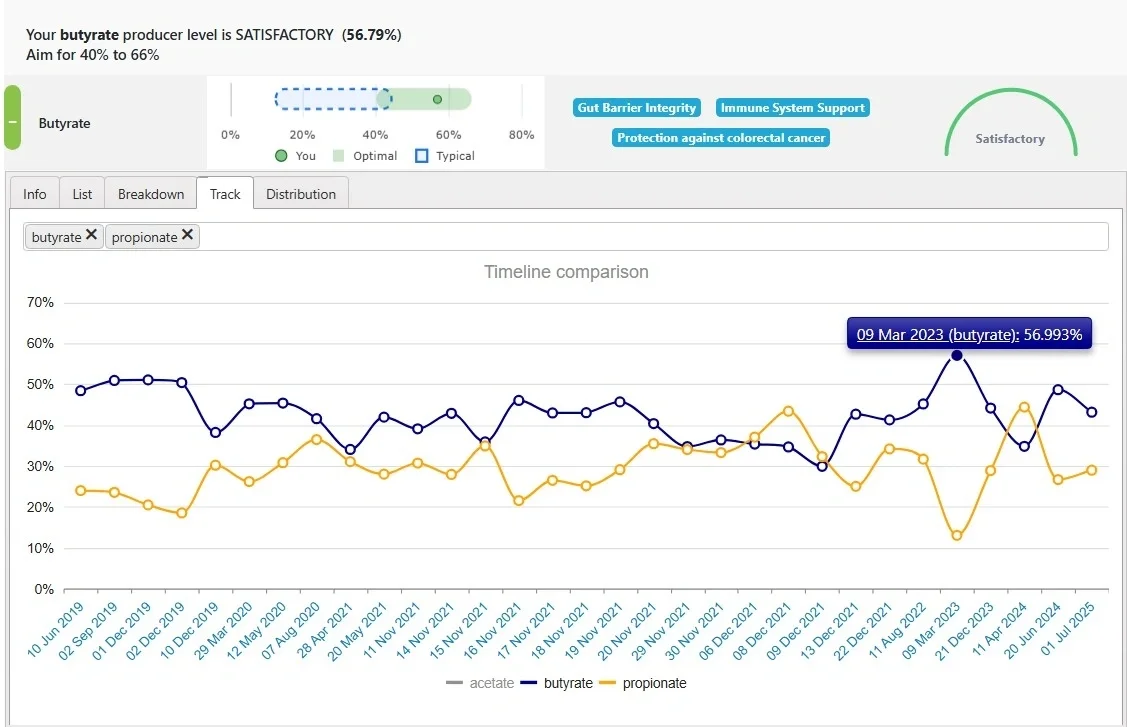
Testing your microbiome gives you a snapshot of what’s happening inside your gut — which species are thriving, which are struggling, and how balanced the overall community is. Tracking it over time helps you see whether your diet, supplements, or lifestyle changes are truly supporting your gut recovery.
Some of the key trends we look for:
Greater microbial diversity — a more resilient ecosystem.
Reduced Proteobacteria — a group linked to inflammation and “gut stress”.
Rebound of keystone species like Faecalibacterium prausnitzii, Bifidobacterium longum, and Akkermansia muciniphila.
Better balance of short-chain fatty acid producers that nourish your gut lining.
Lower markers of dysbiosis or overgrowth (such as Klebsiella or E. coli).
In other words — we’re not chasing perfection, we’re tracking progress and stability.
When to Re-Test
There’s no single timeline that fits everyone, but here’s a general guide based on scenarios we see:
1. After starting a microbiome-focused plan:
Retest at 3 months. The gut typically needs several bacterial “life cycles” to stabilize after major diet or supplement changes.
2. If symptoms are improving or you’re maintaining your microbiome:
Retest every 6 months. This helps track maintenance and catch early shifts before a relapse.
3. If symptoms persist or worsen / troubleshooting:
Retest at 3 months. This helps identify new imbalances, such as bacterial overgrowth or inflammation.
If no major inflammatory imbalance is present but symptoms continue, external factors may be involved:
Poor tolerance to fiber may indicate SIBO or carbohydrate malabsorption.
Poor response to polyphenol-rich foods or herbs may suggest compromised detox pathways (e.g., salicylate or phenol pathways). Retesting can help troubleshoot these issues.
Lack of growth of Bifidobacterium and Lactobacillus despite targeted treatment may indicate the presence of a stronger factor that is reducing their growth. For example, the use of certain medications or the presence of mold toxins.
4. After antibiotics, herbal antimicrobials, or major illness:
Wait 8–12 weeks to allow the microbiome to recover for a more accurate baseline.
Exception: if antimicrobials were used intentionally to target a specific overgrowth, you might retest 2–3 weeks post-treatment to confirm clearance.
Tip: Microbiome shifts happen gradually — like a forest regrowing after a storm. Testing too soon can give misleading results, while waiting too long may miss early patterns worth correcting.
What to Expect When You Re-Test
Don’t be discouraged if your second test doesn’t look “perfect.” Microbiome restoration happens in phases:
Early Phase (0–3 months): Inflammation-linked bacteria like Proteobacteria may still be elevated as the gut barrier heals.
Stabilization Phase (3–6 months): Diversity and beneficial species begin rebounding; symptoms often improve.
Resilience Phase (6–12 months): The gut ecosystem becomes more self-sustaining and less reactive to food or stress triggers.
Even subtle improvements — like higher butyrate producers or fewer inflammatory bacteria — are meaningful signs that your gut is rebuilding.
Why Re-Testing Matters
Without retesting, it’s easy to assume a protocol is working (or not) based purely on symptoms. Microbiome data often reveal subtle changes beneath the surface — sometimes positive trends appear before you feel them.
Re-testing can:
Confirm your approach is moving in the right direction.
Allow fine-tuning of diet or supplements.
Build accountability and motivation — you can see the difference you’ve made.
The Big Picture
Your microbiome is dynamic. It changes with your meals, stress, sleep, and even the seasons. Testing every few months offers valuable insight — not as a scorecard, but as a guide.
When you understand your microbiome’s strengths and weaknesses, you can make informed choices that truly support long-term gut health.
Categories: re-testing tracking Tags: re-testing tracking
